ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2012) Volume 23, Issue 3
Unsafe Injections: A Potential Risk for HIV Transmission in India.
1Department of Microbiology, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
2Department of Statistics, Lucknow University, Lucknow, Uttar Pradesh, India
3Department of Pathology, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
4Department of Medicine, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
5Department of Biochemistry, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
- *Corresponding Author:
- R.K. Singh
Department of Biochemistry SGRRIM&HS, Patel Nagar, Dehradun – 248001
(Former Senior Professor and Head, Department of Biochemistry
Chhatrapati Shahuji Maharaj Medical University, Lucknow 226003), India.
Accepted date: April 07 2012
HIV infection is the most serious public health problem, leading to increased morbidity and mortality worldwide. There are many risk factors contributing to the transmission of HIV infection. Our aim was to study several possible risk factors to which an HIV positive population has been exposed. A total of 350 HIV-positive patients attending the ART Centre and the ICTC of Chhatrapati Shahuji Maharaj Medical University, Lucknow were enrolled in the study, after obtaining informed consent. A detailed history of exposure to various risk factors was recorded by direct questioning. 217/350 (62%) HIV positive patients were males and 133/350 (38%) females. Mean age of the patients was 32.2±10.4 years. Exposure to unsafe/ unsterile injections was the most common risk factor for HIV transmission in 81.7% patients followed by unprotected heterosexual contact in 57.7%, tattooing in 26.6%, blood transfusion in 13.4%, mother-to-child in 6.6% and injection drug use in 1.1%. Our study reports the presence of more than one risk factor for HIV acquisition in a patient and emphasizes that minor risk factors for HIV transmission should not be ignored in the presence of high-risk sexual exposures. General public still needs to be informed about the possibility of HIV transmission by unsafe injections and they should be given more right to choose safe injections for them. Efforts should be made to educate health care workers about safe injection practices to avoid a possible risk for HIV transmission in India.
Keywords
HIV, risk factors, heterosexual transmission, unsafe injections, tattooing, India
Introduction
Since the first detection of acquired immunodeficiency syndrome (AIDS) cases in 1981 among homosexuals in USA [1], the numbers of human immunodeficiency virus (HIV) positive individuals and AIDS cases have increased tremendously. In India, the first evidence of HIV infection in sex workers in Chennai, Madurai and Vellore was obtained in 1986-1987 [2,3]. Since then, there has been an explosive increase in HIV transmission which led to a very rapid growth in the numbers of HIV positive persons and AIDS cases. Currently, it is estimated that about 2.5 million people are living with HIV in India [4]. In India, the HIV epidemic while first detected in specific populations with higher risk of exposure to HIV, such as female sex workers, truck drivers, and injecting drug users (IDU), infection has now been spreading from high risk to low risk populations and from urban to rural areas [5,6,7,8,9].
A majority of HIV infections are reported to occur due to unprotected heterosexual contact followed by mother-to-child transmission and intravenous drug use [10]. Several other risk factors are reported to contribute to the transmission of HIV infection in India, such as reuse of unsterilized syringes [11], needles [12] and tattooing [13]. Most studies derive the risk factors from the likely source of exposure amongst possible risk factors [14,15,16,17,18,19]. In the present study, several possible risk factors to which an HIV positive population has been exposed were analyzed.
Material and Methods
The study was conducted in the Department of Microbiology of Chhatrapati Shahuji Maharaj Medical University (C.S.M.M.U.) Hospital, Lucknow, Uttar Pradesh, India. Uttar Pradesh is a low prevalence state but defined as highly vulnerable state for HIV/AIDS. C.S.M.M.U. is a state-run teaching hospital located in the capital city of India’s most populous state - Uttar Pradesh. The hospital caters mostly to the poor and severely ill patients from the Lucknow city and district and surrounding districts. Patients are mostly referred from primary health centres, district hospitals, nursing homes, private doctors and community health workers. The hospital has an active Anti-Retroviral Therapy (ART) Centre and an Integrated Counselling and Testing Centre (ICTC) facilities. ART Centre and ICTC are well attended and provide counselling and HIV testing and linkages for medical and psychosocial care for persons living with HIV infection. Patients referred from other health care centres are retested for HIV at the ICTC of our centre, as per National AIDS Control Organization guidelines.
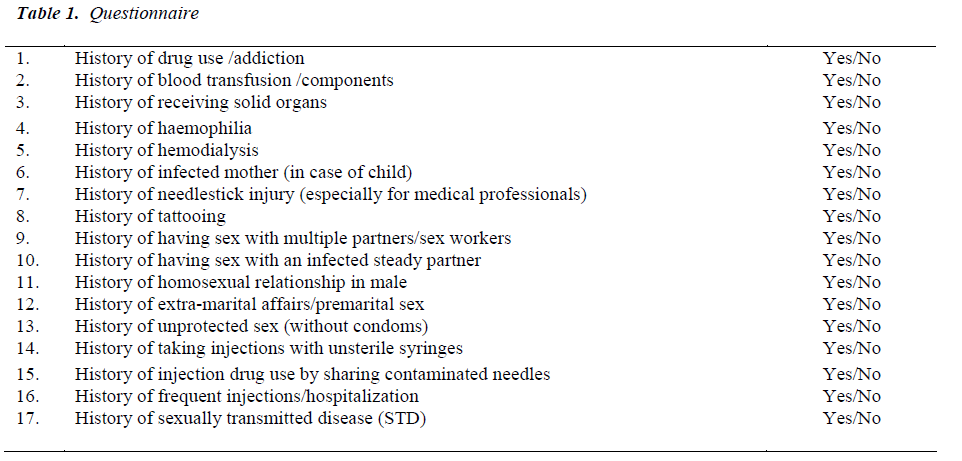
Ethics Committee of C.S.M.M.U. provided ethical clearance for the study. A total of 350 HIV-positive patients attending the ART Centre and the ICTC were enrolled in the study between January 2007 and July 2008, after obtaining informed consent. The patients were interviewed using a pre-designed proforma (Table 1). A detailed history of exposure to various risk factors was taken by direct questioning by the interviewer, using a checklist. A detailed history of exposure for any unsafe injection practices where sterility of the syringe was not assured was also taken. History of tattooing was supported by physical verification of tattoo. The questions were designed so that answers were obtained in a yes or no format. Questions were asked in the local language and responses recorded.
Data was entered in Microsoft Excel. Statistical analysis was performed using SPSS software for Windows (version 16.0, SPSS). Differences in distribution of categorical variables were analyzed using chi-square test. A pvalue <0.05 was considered statistically significant.
Results
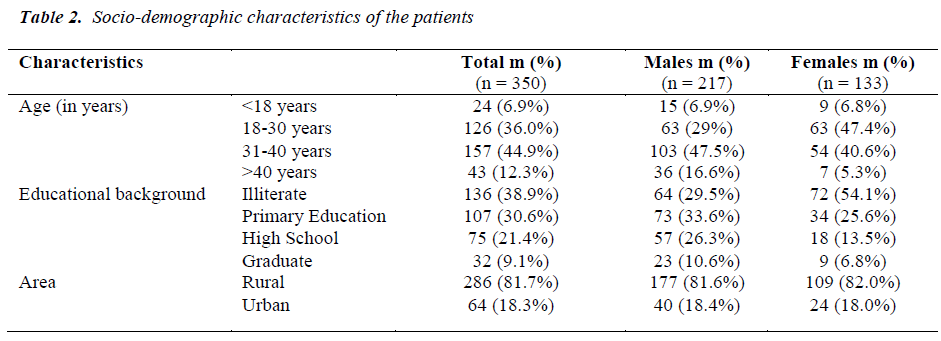
The socio-demographic characteristics of the study population are given in Table 2. 217/350 (62%) HIV positive patients enrolled were males and 133/350 (38%) females. Mean age of the patients was 32.2±10.4 years. Most of the patients were found in the 31-40 years age group followed by the 18-30 years age group. Majority 136 (38.9%) of the patients were illiterate with no formal education, while the 107 (30.6%) had only received a basic primary education. Most (81.7%) of the patients were from a rural background.
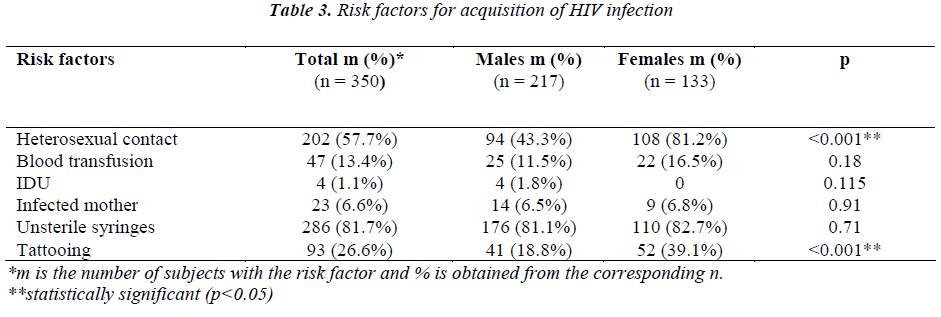
Table 3 describes the exposure to various risk factors in the study population. History of unprotected heterosexual contact was considered if patient gave history of sexual contact with infected spouse or had non-marital sexual partners or multiple sexual partners including female sex workers. 57.7% patients had a history of unprotected heterosexual contact. 94 of the male patients had a history of having sex outside their marriage with commercial sex workers or with infected steady partner or with both, while all 108 of the female patients who acquired HIV infection had sex with their already infected husbands. 13.4% patients had a history of blood transfusion, 1.1% were injection drug users (IDUs) and 6.6% children were born to infected mothers. 81.7% patients had a history of receiving injections with unsafe/unsterile syringes and 26.6% had a history of tattooing. Several individuals reported being exposed to more than one risk factor. 21 (6.0%) patients had a history of unprotected heterosexual contact and blood transfusion, while 1 (0.3%) had a history of unprotected heterosexual contact and injection drug use. None of the patients had a history of being homosexual. None of the patients had a history of haemodialysis or organ transplantation, haemophilia and needlestick injury. None of the patients had a history of sexually transmitted disease (STD).
Discussion
In the present study, several possible risk factors to which an HIV positive population has been exposed were analyzed.
The demographic profile of HIV positive patients at our centre appears to be broadly similar to that reported from other parts of the country [16,17,19].
Estimation of risk factors for HIV acquisition is based on information gathered from HIV infected clients detected during voluntary testing or from surveillance data. In both situations the client is asked to choose from a list of possible risk factors usually with the counsellor or health care worker conducting the interview often guiding the choice. Data entered often tends to be biased towards commonly perceived modes of transmission of HIV in the community. Little data is usually generated on the ‘other’ risk factors including tattooing and unsterile injections. These lacunae have been previously highlighted [20].
In this study, exposure to each risk factor was determined by specific questioning from a long list. Minor risk factors for HIV transmission were not ignored in the presence of high-risk sexual exposures. Several individuals reported being exposed to more than one risk factor.
Unsafe heterosexual contact was a likely risk factor in 57.7% patients in the present study. Unsafe heterosexual contact has been considered by other workers from 56.3% to 93% [17,18]. Blood transfusion was a likely risk factor in 13.4% patients [16], mother-to-child in 6.6% [17] and injection drug use in 1.1% [19]. The proportion of unprotected heterosexual contact in female patients was (81.2%), which is significantly higher (p<0.001) than that in male patients (43.3%). One of the reasons may be that unlike women, the men had exposure to different sources of unprotected sex. Most of the female patients acquired HIV infection through their already infected husbands, who in turn got it from commercial sex workers, similar to other studies in India [8,14,19]. Married women do not have sufficient understanding of risk of HIV from their spouses due to poor educational background. This is also because women have very little say in decision making, like condom use with their partners, especially if she is economically dependant on her husband. Although the proportion of transfusion associated AIDS fell after the Supreme Court ruling made HIV testing of all blood bottles mandatory in 1999, but still there are few reports on blood donors which showed that the percentage of seropositivity for HIV was significantly higher in replacement donors. [21,22,23,24].
Exposure to unsafe/unsterile syringes was the most common risk factor in 81.7% patients in this study. Similar trends are observed in other studies from other parts of India [11,12,25]. One of the reasons may be that most of the men lie about their heterosexual contact with commercial sex workers. Also in the organized health centre, untrained health service providers and other such practitioners in rural or urban slum areas continue the procedure of using unsafe injections and people receive those injections without any hesitation. This shows that the extent of understanding and awareness about HIV transmission is still insufficient, even among practitioners and also among general public. Tattooing was a likely risk factor in 26.6% patients [13]. The proportion of tattooing in female patients was (39.1%), which is significantly higher (p<0.001) than that in male patients (18.8%). The reason may be that in rural areas, most of the females get tattoo on their hand after marriage due to a locally prevalent
Conclusion
The present study highlighted the presence of more than one risk factor for HIV acquisition in a patient. While the reporting of more than one risk factor may appear to add confounders in estimation of risk factors, identifying of all risk factors help to define the relative importance of all modes of transmission in the community, thereby helping to contain the epidemic. Exposure to unsafe/unsterile injections was the most common risk factor observed in the present study followed by heterosexual contact, tattooing, blood transfusion, mother-to-child and injection drug use. This highlights that while the major risk factors may be the main routes of HIV transmission in the community, use of unsafe injections may play some role in sustaining HIV epidemic in India. While there are widespread use of Media and Information Education and Communication (IEC) especially to reduce risk factors like heterosexual contact and mother-to-child, strong government programs for awareness about unsafe syringes and HIV transmission are still required. Implementation of safe injection practices at all levels of health care settings is urgently needed.
Acknowledgements
The authors would like to thank Prof. U.K. Misra, Senior Professor and Head, Department of Neurology, and Dean, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, for his guidance, consistent patronage and support and for reviewing the manuscript. This study was funded by the Uttar Pradesh Council of Science & Technology, Lucknow.
References
- CDC. Pneumocystis pneumonia - Los Angeles. MMWR 1981; 30: 250-252.
- John TJ, Babu PG, Jayakumari H, Simoes EAF. Preva- lence of HIV infection among risk groups in Tamil- nadu, India. Lancet 1987; 17: 160-161.
- Simoes EA, Babu PG, John TJ, Nirmala S, Solomon S, Lakshinarayana CS et al. Evidence for HTLV-III infec- tion in prostitutes in Tamil Nadu (India). Indian J Med Res 1987; 85: 335-338.
- National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India: HIV estimates in India. 2006.
- Solomon S, Kumarasamy N, Ganesh AK, Amalraj RE. Prevalence and risk factors of HIV-1 and HIV-2 infec- tion in urban and rural areas in Tamil Nadu, India. Int J STD AIDS 1998; 9: 98-103.
- Mehendale SM, Rodrigues JJ, Brookmeyer RS, Gan- gakhedkar RR, Divekar AD, Gokhale MR, et al. Inci- dence and predictors of human immunodeficiency virus type 1 seroconversion in patients attending sexually transmitted disease clinics in India. J Infect Dis 1995; 172: 1486-1491.
- Mehendale SM, Shepherd ME, Divekar AD, Gangakhedkar RR, Kamble SS, Menon PA, et al. Evidence for high prevalence & rapid transmission of HIV among individuals attending STD clinics in Pune, India. Indian J Med Res 1996; 104: 327-335.
- Gangakhedkar RR, Bentley ME, Divekar AD, Gadkari D, Mehendale SM, Shepherd ME, et al. Spread of HIV infection in married monogamous women in India. JAMA 1997; 278: 2090-2092.
- Bollinger RC, Brookmeyer RS, Mehendale SM, Paran- jape RS, Shepherd ME, Gadkari DA, et al. Risk factors and clinical presentation of acute primary HIV infec- tion in India. JAMA 1997; 278: 2085-2089.
- National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India: An- nual Report 2009-10.
- Kotwal A, Priya R, Thakur R, Gupta V, Kotwal J, Seth T. Injection practices in a metropolis of north India: perceptions, determinants and issues of safety. Indian J Med Sci 2004; 58: 334-344.
- Kermode M, Holmes W, Langkham B, Thomas MS, Gifford S. Safer injections, Fewer injections: injection safety in rural north India. Trop Med Int Health 2005; 10: 423-432.
- Panda S, Kumar MS, Lokabiraman S, Jayashree K, Satagopan MC, Solomon S et al. Risk factors for HIV infection in injection drug users and evidence for on- ward transmission of HIV to their sexual partners in Chennai, India. J Acquir Immune Defic Syndr 2005; 39: 9-15.
- Kumarsamy N, Solomon S, Jayaker PSA, Vnilla R and Amalraj RE. Spectrum of opportunistic infections among AIDS patients in Tamil Nadu, India. Int J STD AIDS 1995; 6(6): 447-449.
- Sircar AR, Tripathi AK, Choudhary SK and Misra R. Clinical profile of AIDS: a study at a referral hospital. J Assoc Physicians India 1998; 46(9): 775-778.
- Kothari K and Goyal S. Clinical profile of AIDS. J Assoc Physicians India 2001; 49: 435-438.
- Zaheer MS, Rabbani MU, Ahmad Z, Khan T, Rewari BB and Pandey DK. Clinical and demographic profile of patients of AIDS in and around Aligarh. JIACM 2003; 4(2): 121-126.
- Kumarasamy N, Solomon S, Flanign TP, Hemlatha R, Thyagarajan SP and Mayer KH. Natural history of Human Immunodeficiency virus disease in southern India. Clin Infect Dis 2003; 36: 79-85.
- Chakravarty J, Mehta H, Parekh A, Attili SV, Agrawal NR, Singh SP et al. Study on Clinico-epidemiological Profile of HIV Patients in Eastern India. J Assoc Physicians India 2006; 54: 854-857.
- Correa M and Gisselquist D. Routes of HIV transmis- sion in India: assessing the reliability of information from AIDS case surveillance. Int J STD AIDS 2006; 17: 731-735.
- Kamat HA, Banker DD, Koppikar GV. Human immu- nodeficiency viruses types 1 and 2 infection among re- placement blood donors in Mumbai (Bombay). Indian J Med Sci 2000; 54: 43-51.
- Garg S, Mathur DR, Garg DK. Comparison of sero- positivity of HIV, HBV, HCV and syphilis in replace- ment and voluntary blood donors in western India. Indian J Pathol Microbiol 2001; 44: 409-412.
- Singh B, Verma M, Kotru M, Verma K, Batra M. Pre- valence of HIV and VDRL seropositivity in blood do- nors of Delhi. Indian J Med Res 2005; 122: 234-236.
- Pahuja S, Sharma M, Baitha B, Jain M. Prevalence and trends of markers of hepatitis C Virus, hepatitis B virus and human immunodeficiency virus in Delhi blood do- nors: A hospital based study. Jpn J Infect Dis 2007; 60: 389-391.
- Lakshman M, Nichter M. Contamination of medicine injection paraphernalia used by registered medical practitioners in south India: an ethnographic study. Soc Sci Med 2000; 51: 11-28.